I see I left off on Day 2 of our admit last week?? Well, now I'm going to have to back-track a bit because this morning we are home from the hospital for the SECOND time in the past 8 days. I would have updated throughout the admissions, but Elise had custody of my laptop for the majority of the time, and I choose my battles carefully.
Ok. So last Friday, November 14, shortly after I posted my last update, the liver team came in initially with some less-than-great news but same as I had been told in the ER-- "not much to do except manage the symptoms of RSV and monitor and protect her liver." Well, I expressed to Dr. Sonny that it was so upsetting that there was no actual treatment to help her get over the RSV, and I asked whether it might be appropriate to consult infectious disease team, as I know Dr. Munoz has been very helpful in the past with Elise.
 |
| Dr. Sonny Harpovat (attending hepatologist) with Elise |
I didn't get the impression that they took my commentary during rounds really seriously, but….. ASK AND YOU SHALL RECEIVE!! About an hour later, the liver team and infectious disease teams, led by Dr. Sonny and Dr. Munoz, descended on our room. We were in an isolation room, so I could hear them in the dressing area right outside our door, and I was thinking to myself, "OMG, what else has come back positive that we're about to have to deal with.?" Dr. Sonny came in w/ the hugest smile on his face….and he said, "Erin, this is important since we dressed out again…We have a new and very good plan….but a personal question too….are you pregnant or do you plan to become pregnant in the next 6 months?" I almost wanted to LOL at him, but given the situation, a simple "No," and "No" sufficed. The plan? RIBAVIRIN. Ribavirin would be an inhalation medication administered in an isolation tent for 2 hour treatment sessions, 3 times/day, for 3 days. Dr. Munoz stepped in at this point and answered my questions regarding the risks vs benefits. They all agreed that this medication would not harm Elise and could only help. The only risk would be to developing fetus, so no one exposed to the treatment should be pregnant or become pregnant within 6 months. The team indicated that Ribovarin is rarely used at TCH because of the strict criteria to use it for RSV, and it is super expensive, so insurance coverage had to be verified. Dr. Munoz stated that although she has not used Ribavirin for RSV since 1995, they would be keeping Elise inpatient for at least 3 days at the rate things were going anyway, so at least the use of Ribavirin would allow us to be ATTACKING and killing off the RSV rather than just monitoring and treating the symptoms. And so I agreed to start Ribavirin, and the respiratory therapists came in to set up the tent treatment by 1:00 pm that day.


Elise began responding wonderfully to the Ribivirin almost immediately following her first treatment. She started talking and smiling and showing interest in eating and drinking. So much so that when she asked for chicken nuggets, I was motivated to run across the street in dress boots and sweat pants to get her a "Happy Meal."
 |
| "Happy Meal' makes things happier! |
On Day 3, November 15, I was starting to get "cabin fever" in that room. Thankfully, David relieved me that evening so that I could go to our good friends' and fellow liver family's annual fundraiser event benefiting pediatric liver disease research conducted at Texas Children's Hospital and Children's Hospital of Atlanta. I had a wonderful time visiting with our liver family….love them all so much…..they truly keep me sane much of the time in "Liverland."
 |
| "Liver Family"… from left to right….me, Ben, Troy, Kelli, Tara, Hal, and Jennifer. |
 |
| LIVER MOMS! Jennifer, Tara, me, and Harriet :-) |
David had "tent duty" that night while I was away. I was so anxious to see how he would deal with 2 hours inside that tent with Elise. I was utterly shocked when he texted me the following picture. Not sure if it's the advanced practice nurse inside him or the mechanical genius….but he managed to keep Elise calm breathing through the mask without being inside the tent with her.
 |
| David on "tent duty." Notice he is not inside the tent. Good for him, I suppose. I was not able to negotiate that. |
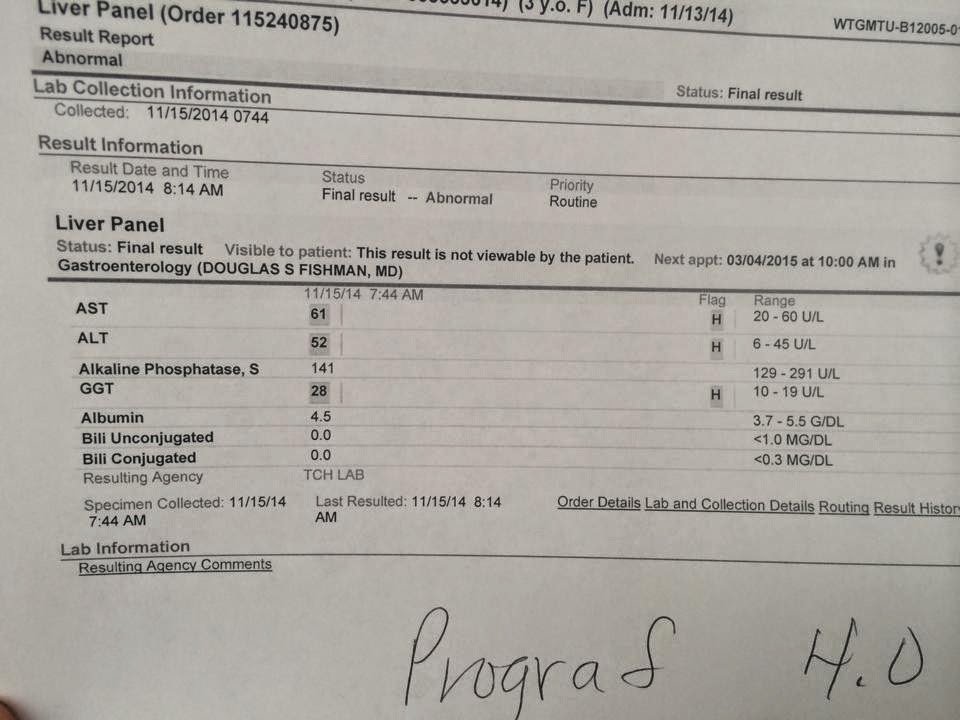
In other news, on November 15, I was pleased to lay my eyes on fastastic-looking liver panel. And I could have sent a fruit basket to our nurse for actually printing it for me. Because….let's be real for a second….I KNOW it CAN be printed. But I seem to always get these nurses that tell me they can't print it, leaving me to wait until rounds to find out about Elise's liver numbers. Anyway, if I haven't said it before, I LOVE our liver team….they are BRILLIANT. When we went to liver clinic on 10/20/14, Dr. Fishman noted her elevated numbers but suspected a brewing virus. Now, the virus was identified, and we were attacking it, and her liver was beautiful and happy!!! :-)
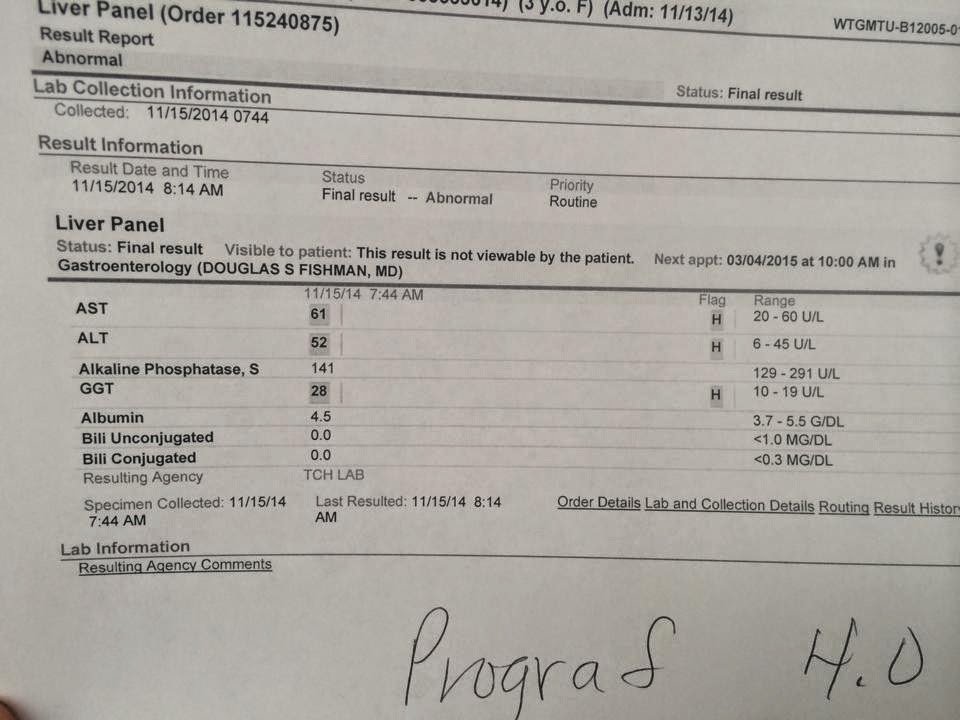 |
| liver panel, November 15 |
November 16…..Elise was doing so much better….continuing Ribavirin treatments but really ready to bust out of there.
November 17….Day 5….our primary attending liver doc, Dr. Fishman, and Dr. Munoz with the infectious disease team rounded bright and early. Elise got a thorough once-over by everyone. According to Dr. Munoz, "Elise got our special treatment because there was the potential or things to go very bad….but she came in at exactly the right time for the Ribavirin to work." And with that, were were DISCHARGED home, with instructions to follow up for repeat labs on Thursday 11/20. And a final order by Dr. Fishman was to decrease Elise's prograf (immunosupresent) to 0.25 mg twice/day in order to allow her body's immune system to do it's job and clear itself completely of any lingering virus or infection.
 |
| Dr. Fishman (standing,) and Dr. Munoz (kneeling) with Elise during rounds |
Ethan and Elise were so happy to be reunited on Monday night. They played together until about 10:00 pm. Elise continued to look GREAT on Tuesday and Wednesday. I resumed my work, with no reason to think that all was not well (remember, I do maintain a full-time job as a clinical social worker/ Care Advocate outside of "Liverland.")


This past Thursday, November 20, I woke Elise up at 6:00 am for our scheduled labs, and Elise sat up in bed and declared, "I not feel good." Her face was red, and her body felt warm. I checked her temperature which was 101.7. Surely, this couldn't be. I hoped that it was just a fluke….maybe she had a nightmare overnight and got overheated similar to what I was experiencing at that particular moment. Since she really didn't have any other symptoms at that point, I gave her a dose of Tylenol and figured I would continue to monitor her, and if things got worse, we'd be at TCH for labs in a bit anyway. So we got dressed, jumped in the car, and we were on our way.
As we sat in the lab waiting area, I could feel that Elise's fever had not broken, and I noted that she was breathing hard. I checked her pulse and started counting her respirations; she was tachicardic and breathing very fast. Her labs were drawn quickly, and the phlebotomist also noted that she didn't look very good. It was all I could do not to request that they draw an extra couple of vials, as I anticipated that we would soon be in need of blood cultures. As soon as we left the lab, I called Elise's transplant coordinator, Sarah, and asked if she could come down and "eyeball her" to see if there's really any concern or if I'm just overreacting. Sarah wasn't happy with how Elise looked and re-routed us from the elevator lobby to a 3rd floor seating area and asked us to stay put there until she had a chance to review Elise's labs and speak with Dr. Fishman. It seemed like just minutes later, my cell phone rang, and Sarah was on the other end telling me that Elise's WBC (white blood cell count) was 20--very high, indicating infection-- and so Dr. Fishman wantd us down in the ER for a full medical workup.
Well, I sat there in disbelief for a second. I had nothing with me in preparation for an ER visit or admission. David was at work and would be stuck there until 8:00 pm, after daycare closes. I had no plan for Ethan. I was expected to be working that day too. So, I started doing what I could do to keep things together. On our way to the ER, I stopped with Elise in the gift shop and let her pick out a toy to keep her entertained in the ER. And I got myself a coffee. I called my manager and team lead and told them I would not be able to be at work, and I called HR to report an intermittent absence on my FMLA case.
We arrived in the ER, which was overflowing. Thankfully, Dr. Fishman had called ahead for us, and we didn't have to sit down waiting area or even in triage; we were taken straight back to an ER exam room, and following an initial exam, Elise was promptly placed on "shock protocol." Several nurses came in and simultaneously began working to establish an IV access, draw labs and cultures, and to start IV fluids and antibiotics. I pointed out that we had just gotten labs drawn within the hour, so although they did have to stick her again for additional labs needed, they didn't repeat anything unnecessarily. This was not my first rodeo, but I listened as the nurse explained to me that Elise was being treated w/ shock protocol to treat for or prevent septic shock based on her fever and elevated blood pressure, pulse, respirations.
 |
| in the ER….again…. |
Liver team admitted Elise to the 12th floor again. Apparently a fever and WBC of 20, being immunosupressed, gets you a ticket to a room with a view. Chest x-ray looked good, urinalysis was negative, and ears/ throat looked good, so the plan was to try and identify the source of infection, and until then continue treatment with the IV antibiotic Zosyn and IV fluids. Shortly after we arrived on the floor, Dr. Fishman came by and told me that her liver is still looking good, and that they would be monitoring her liver very closely to make sure it tolerating lowered Prograf doses. Also, he indicated that he'd be requesting some consults with other specialties such as pulmonology, immunology, and infectious disease, and possibly immunology to get their opinion and recommendations. By the time Dr. Fishman came to see her, she had already received a couple of rounds of IV Zosyn and fluids, and her temperature and vitals were stabilized, which was great news, and said this was very encouraging.

By the next morning, yesterday, November 21, Elise looked 100% better. There was still no answer as to the source of the infection, but whatever it was seemed to be under control. For whatever reason, Elise was being kept on "contact precautions" meaning she could not leave the room, but she was making it clear that she wasn't having that. Dr. Fishman said during rounds that he still wanted pulmonologist to see her, and he wanted her to get additional doses of IV Zosyn, but he felt that she could probably be safely discharged by the end of the day.
 |
| "gonna make a run for it!" |
The pulmonology team came in around 2 pm, and they recommended that we increase her daily inhaled steroid, Qvar, to 2 puffs (160 mg) twice daily. They also reviewed the previous pulmonology notes from April and said it might be appropriate to consider a bronchoscopy soon to evaluate whether there is an underlying airway issue secondary to her history of numerous intubations. Dr. Fishman concurred but stated that if we were to take her to OR and place her under anesthesia for a bronchoscopy, they would want to get ENT on board to come in and re-insert her ear tubes at the same time, because Elise's ear tubes are noted to no longer be sitting in hear ear canals, and this of course places her at risk of ear infections again. And Lord knows we don't need that. David asked his routine questions about the anesthesia, and we all agreed that IF she were to put a brochoscopy on the books, it should be done along with another procedure that is actually medically necessary (i.e. ear tubes) rather than "just to look around."
We are now back home again, and we are to follow up for labs at TCH on Tuesday morning 11/25/14. I swear…we're going to be in and out of there so quick, I won't even get charged for parking. LOL. Seriously. I've had enough of the hospital routine for a while. So happy to be home, and we are so ready for the holidays!! :-)
 |
| Adios, TCH!!! (take 2!) |














No comments:
Post a Comment